| Nosology |
Characteristic syndromes/symptoms |
Differentiation test |
| chronic prostatitis |
The average age of patients was 43 years old.Pain or discomfort in the pelvic area that lasts 3 months or longer. The most common site of pain is the perineum, but discomfort may also occur in the suprapubic and pelvic inguinal areas, as well as in the scrotal, rectal, and lumbosacral areas. Pain during and after ejaculation.Voiding dysfunction usually presents with symptoms of irritation and, less frequently, symptoms of bladder outlet obstruction. |
During - you can detect swelling and tenderness of the prostate and sometimes enlargement and smoothness of the median sulcus. For differential diagnosis, the condition of the rectum and surrounding tissues should be evaluated.Prostatic secretion - Determine the number of leukocytes, lecithin granules, amyloid bodies, Trousseau-Lalerman bodies, and macrophages.Bacteriological studies were performed on prostate secretions or urine obtained after massage. Based on the results of these studies, the nature of the disease (bacterial or nonbacterial prostatitis) is determined.Diagnostic criteria for bacterial prostatitis- The third portion of urine or prostate secretion contains bacteria of the same strain with a titer of 103 CFU/ml or higher, provided the second portion of urine is sterile.
- Bacterial titers in urine or prostate secretions increased tenfold or more in part III compared with part II.
- Part III urine or prostate secretions contain more than 103 CFU/ml of true urinary tract pathogenic bacteria, unlike other bacteria in Part II urine.
Prostate ultrasonography has high sensitivity but low specificity for chronic prostatitis. The study allows not only differential diagnosis but also identification of the form and stage of the disease and subsequent monitoring throughout treatment. Ultrasound can assess prostate size and volume, echogenicity |
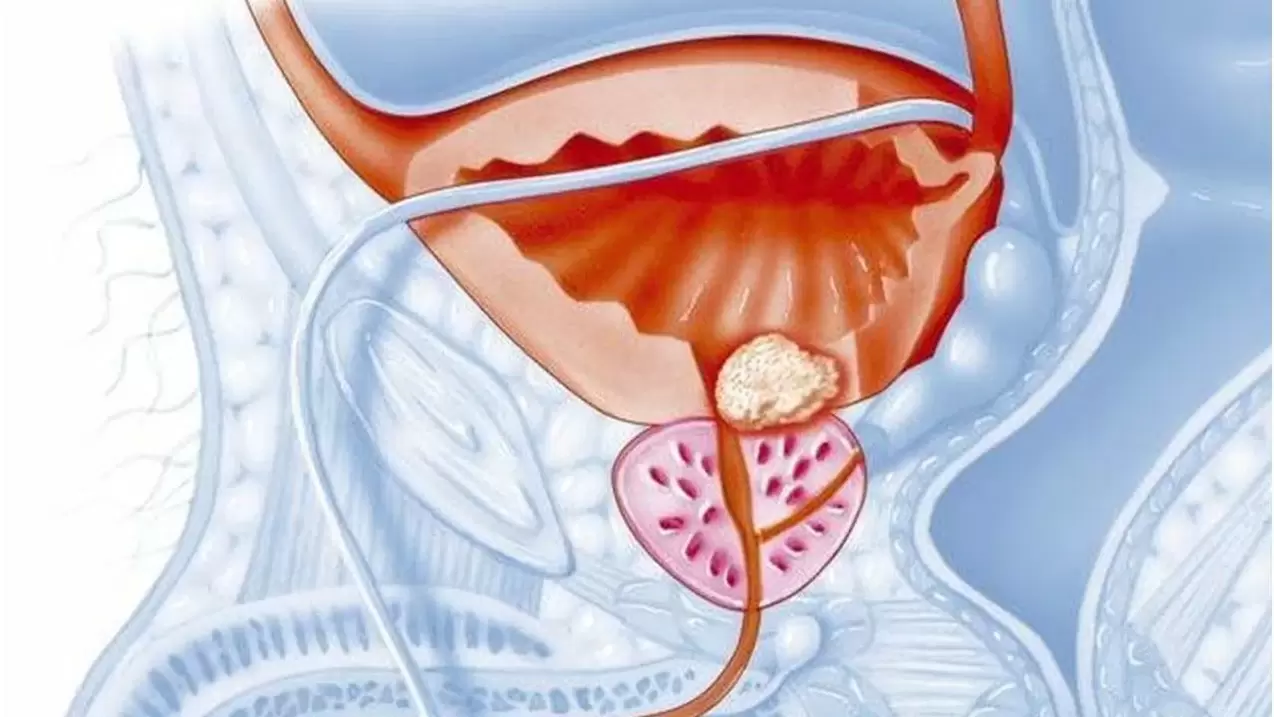
| Benign prostatic hyperplasia (prostatic adenoma) |
This condition is more common in people over 50 years old. Urination gradually increases and urinary retention slowly increases. Increased frequency of urination at night is typical (in chronic prostatitis, increased frequency of urination during the day or early morning). |
PRI - The prostate is painless, enlarged, elastic, has a smooth central sulcus and a smooth surface.Prostatic secretion - the amount of secretion increases, but the number of leukocytes and lecithin granules remains within the normal physiological range. The secretion reaction is neutral or slightly alkaline.Ultrasound - Bladder neck deformation was observed. The adenoma appears as a bright red mass extending into the bladder cavity. There is significant proliferation of glandular cells in the cranial part of the prostate. The structure of adenomas is uniform, with regularly shaped darkened areas. The glands are enlarged in the anteroposterior direction. In fibroadenoma, bright echogenicity from connective tissue can be detected. |
| prostate cancer |
People over the age of 45 are affected. The location of pain is the same when diagnosing chronic prostatitis and prostate cancer. Prostate cancer pain in the waist, sacrum, perineum, and lower abdomen may be caused by lesions in the gland itself and metastases in the bones. Rapid development of complete urinary retention often occurs. Severe bone pain and weight loss may occur. |
IF - Identifies a single node of cartilage density or a patchy dense infiltrate throughout the prostate that is limited to or spreads to surrounding tissue. The prostate is immobile and painless.PSA - more than 4. 0 ng/mlProstate biopsy - identifies collections of malignant cells in the form of ductal casts. Atypical cells are characterized by hyperchromasia, polymorphism, variability in nuclear size and shape, and mitotic figures.Cystoscopy - A pale pink mass is found in a ring around the bladder neck (result of infiltration of the bladder wall). The mucosa is often swollen and congested, and epithelial cells proliferate malignantly.Ultrasound - asymmetry and enlargement of the prostate, its marked deformation. |